
As the spores multiplyThe fungus can spread to the skin of the feet and nails, Penetrates into the blood through the microcracks, and flows to all internal organs with the blood.
What kind of fungus grows on the toes?

- Mycosis of the toes is caused by the pathogenic anthropophagus microbe tinea pedis. . .
- Less commonly, the pathogens of the disease are molds and yeast-like fungi of the genus Candida.
- The fungus's favorite habitat is the skin folds between the fingers, where it is warm and moist.
- As the microorganisms multiply, the spores of the microorganisms will also spread under the toes, and then spread to the entire foot.
- The main infections of fungi occur in public places: bathrooms, swimming pools, saunas, gym locker rooms.
- Microorganisms are fully tolerant of low temperatures and excessive drying on the surface. They can last for a long time in clothes, carpets, and shoes, and if given the opportunity, they will adhere to the skin of the feet.
- Transmission of organisms usually occurs within the family, When using general hygiene products, slippers, nail tools.
- After entering the skin, microorganisms can stay dormant for a long time. The active growth of spores begins with the emergence of favorable conditions, that is, the reduced immunity of the infected person
- If the spores adhere to the skin of a person suffering from a chronic disease or who does not observe hygiene rules, the development of mycosis starts almost immediately.
- For patients with chronic diseases, it is particularly important to understand what the fungus on the fingers looks like, because they are more susceptible to pathogens.

- Dysfunction of the endocrine system;
- Poor blood circulation in limbs, Vein tumor;
- flatfoot,Causes skin friction to increase;
- Systemic stress
- Periods of hormonal changes in the body: pregnancy, menopause, puberty;
- Inflammation of the lymphatic system;
- After surgery or traumadecrease in immunity. . .
Sweating feet, shoes made of synthetic materials, and micro-damage of the skin can all promote the growth of fungi.
Inappropriate nutrition creates favorable conditions for the growth of spores: the abuse of sweets, flour, high-fat foods, and alcoholic beverages.
In children, toe fungus is rarely diagnosed. The main cause of fungal disease in children is lack of hygiene.
Symptoms and forms of the disease
Even before the visual signs of fungal disease appear, it is possible to suspect the development of a foot infection in the initial stages.The first signs of infection are skin peeling and itching.. . .
When microorganisms begin to invade the epidermis, the surface of the finger will be covered with small scales and cracks.
An unpleasant smell emanated from the soles of the feet. The specific symptoms depend on the form of the disease:
- deleted.Small cracks and slight peeling appeared under and on the surface of the finger.
- Scaly hyperkeratosis.There was severe itching, burning, and white scabs formed on the fingertips.

- Disorganized.There are skin swelling, redness, moisture formation between the fingers, peeling of the skin, and the formation of deep cracks.
- Sweat smells.It manifests as a rash of small serous vesicles. Severe itching, erosion formed in the place where the bubble broke, and inflammation of the entire foot began.
important! In the later stages of the disease, fungi can penetrate the nail surface and begin to change their color and structure. The nails are covered with colored spots, deformed, and broken.
diagnosis
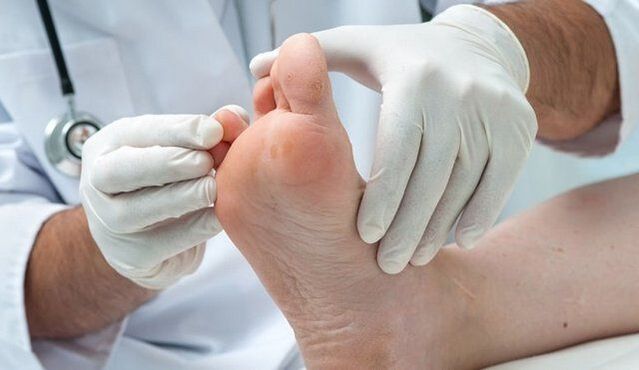
- When the first clinical symptoms of infection appear, it is necessary to consult a doctor for diagnosis.
- Although the symptoms of the fungus are clearly visible even in the photos,Only an expert can identify a specific pathogen.
Laboratory tests are prescribed for patients:
- Microscopic examination of skin particles.
- Bacterial culture of debris and liquid from vesicles.
- DNA research of biological materials.
- blood test.
treatment
- The main activities are ——Thorough skin hygieneIt is also treated with topical antifungal drugs.
- In the later stages of the development of fungal infections, doctors will take antifungal drugs by mouth.
- As an adjunct to drug therapy, folk remedies and physical therapy procedures are used.
- Follow your doctor's advice carefully to cure the fungus on your toes without reducing the time you take prescription medications.
drug
Medication includes the use of two groups of drugs:
- External preparations: ointments, creams, gels, sprays.
- Oral preparations.
important! Comprehensive treatment measures also include special diets, taking immune stimulants, and methods to restore intestinal flora.
physiotherapy
Physical therapy procedures are in addition to medications to accelerate the healing process:
- Ultraviolet rays irradiate the skin. . . The rays penetrate the skin to a depth of 0. 6 mm and kill the fungal spores in it. The duration of the meeting is 15-20 minutes. In the early stages of infection, the use of ultraviolet radiation can avoid the use of antifungal agents.
- Diathermy,Pulse therapy, UHF therapy to improve peripheral circulation.
- Laser irradiation of the skin. . . Skin irradiation can inhibit inflammation, relieve itching, dry and humid areas.
Traditional method

As an aid to medicines, prepared according to folk recipes, they are very effective.
According to the review, effective assistance was provided in the following areas:
- Bath with soda and salt. . . 1 tablespoon. The lake dissolves salt and soda in 2 liters of water and adds 10 drops of iodine. Soak your feet in the solution for 15 minutes. This procedure is performed before applying the antifungal agent.
- Tray with potato skin decoction. . . soak the broth in a broth at the right temperature for 20 minutes, then wash. This procedure is carried out every day until the symptoms disappear.
- Aspen bark decoction tray. . . Pour 100 grams of chopped bark into 500 milliliters of boiling water and hold until it cools. The resulting immersion liquid is added to the bath.
- Garlic ointment. . . 2 large cloves of garlic are pressed into a gruel and mixed with 100 grams of butter. Apply the ointment to the steamed skin for 10-15 minutes a day for one month.
- Decoction applicationMedicinal herbs. A series of chamomile and violet, 2 tablespoons each, pour one liter of boiling water and hold for 2-3 hours. Apply gauze soaked in the infusion solution to the inflamed area for 30 minutes every day.
- Compress with burdock leaves. . . Knock off the fresh burdock leaves with a hammer, wrap the legs, fasten them with bandages, and put on socks. The compressed bag is changed twice a day. The duration of the course is 21 days.
- Carrot juice applicationAnd vinegar. 1 tbsp. Hu mixed carrot juice with 9% vinegar and applied a tampon to the inflamed area.
- Egg vinegar ointment. . . Pour 100 ml of vinegar (70%) into a raw egg for 7 days. Mix the dissolved eggs with 100 grams of butter and stir. The obtained lotion was applied to the steamed legs, wrapped in foil and put on socks. Repeat this procedure every day until the fungus is completely cured.
- Compressed with ammonia. . . Add 1 tablespoon to 200 milliliters of water. Lake ammonia water, moisten the gauze with the solution, wrap your feet in it and put on socks. Compression is done in the evening until morning. The total number of programs is 9-10.
Several interesting recipes for curing fungi. The use of traditional medical methods must necessarily require the permission of the attending physician.
complication

Spread through the body and penetrate into the blood, the infection affects internal organs and negatively affects the function of the entire organism:
- Long-term exposure to mycotoxins can cause allergic reactions, worsening bronchial asthma, and dermatitis.
- Penetrating into the blood can disrupt the work of internal organs.
- Deep fungal diseases can lead to the progression of diabetes, and in its context, it can develop into gangrene and bone infections.
prevention
Organisms with a strong immune system can resist any infectious disease. Therefore, the main measure to prevent fungal infections is to maintain the body's defenses.
Following hygiene rules will help avoid infection with fungal spores:
- DailyChange socks and tights;
- Use breathable shoes made of natural materials;
- Wear special shoes(Slippers, slippers) in public places;
- Foot skin treatmentUse special protective sprays when visiting swimming pools, bathrooms, and beaches;
- pedicureIn a verified salon,Whether the disinfection of the instruments is carried out correctly;
- Try on shoes in the storeIn disposable socks. . . In order to prevent the spores from persisting on various surfaces, it is necessary to disinfect them with a 45% vinegar solution.It is recommended to change towels and slippers.Treat the remaining shoes from the inside with a vinegar solution and put them in a plastic bag for 12 hours.
- Boil sheets, socks, tights, and towels in a soap and soda solution for 10-15 minutes.

Toe fungus should not runTherefore, when the first symptoms appear, it is recommended to consult a doctor.
Starting treatment in time will allow you to respond quickly to the fungus and avoid complications. The fungal disease must be treated until the symptoms are completely eliminated and the skin is restored.
Fungus on little toes: causes, symptoms (photos) and treatments
Fungus on nails or feet always starts with the failure of the outermost toe.
In most cases, the big toe is affected first because it has the largest nail, but in some cases, the fungus appears first on the little toe.
The danger of this onychomycosis lies in the rapid destruction of the nail plate, which is related to the small size of the nail on the little finger.
Causes of disease development

Toenail fungus usually starts with damage to the outer toe
The fungus on the little toes is the result of poor personal hygiene when going to public places. In public showers and swimming pools, fungal spores can adhere to the skin. This is because fungi actively multiply in humid and hot environments.
Another reason for the development of the disease is profuse sweating and microtrauma to the nail plate. In this case, you can get the disease while trying on shoes, using someone else’s towel or nail tools.
The fungus on the little finger of the hand most often occurs from contact with an infected person. Careless handshake will cause spores to enter the nail plate.
The main condition for the development of the disease is the decline of systemic and local immunity. Hyperhidrosis, trauma and injury, circulatory disturbances in the extremities-all these can lead to a decrease in local immunity and increase the risk of infection.
Fungal infection of the pinky finger is characterized by rapid development of the disease. Onychomycosis is caused by fungi that feed on keratin, which is the building material of nails.
The smaller the nail, the faster the pathogenic flora destroys it, destroying keratin, which means that the infection will quickly spread to healthy nails.
If the thumb nail has lesions, the disease progresses slowly, and the symptoms will last for several months. If there is onychomycosis on the little finger, the symptoms will become obvious within a week after the fungal spores enter the nail.
How to recognize the disease?
The characteristic symptoms of fungus on the little finger of the nail depend on the exact location area. The fungus can affect the nails and fingers or the space between the fingers. In the first case, the symptoms are as follows:
- Yellow nails;
- Thickened nail plate;
- The appearance of wrinkles and cracks;
- The nail is severely deformed.
A thick discharge with an unpleasant smell may appear under the nails. The addition of infection is accompanied by purulent discharge. If left untreated, the nail will collapse completely and peel off the nail bed over time.
When the finger skin is affected, the following symptoms will appear:
- Redness of the skin;
- Severe itching;
- Severe peeling
- The appearance of an unpleasant smell.
The fungus on the little finger poses a serious threat to the rest of the healthy finger, because the spores will quickly spread to healthy skin. In advanced cases, the fungus can affect the interdigital space, nail plate and foot skin. All of this is accompanied by severe itching and unpleasant odors on the feet.
diagnosis

If you notice changes in the nail or skin on your little finger, you should see a dermatologist. The doctor will check and take the scrapes for analysis. In the case of skin damage, the flaky scales are sent to the laboratory, and they are easily separated from the skin.
If the nail plate is affected, the doctor will cut a small piece of nail and remove a piece of exudate under the nail plate. This material was sent to the laboratory for microscopic analysis. Based on the research conducted, the best treatment plan is selected.
Treatment principles
To treat the fungus on the little finger, use an external antifungal agent. In order to get rid of this disease faster, you must:
- Monitor personal hygiene;
- Regular foot baths;
- Treat the skin around the affected area with antiseptics;
- Improve immunity.
To avoid the spread of fungal spores to healthy nails, the affected fingers should use a separate manicure tool, preferably a disposable file. The affected area must be treated with special products every day, the skin must be thoroughly cleansed, disinfected, and only socks and shoes made of natural breathable materials must be worn.
medical treatement
In the treatment of foot mycosis and little toe mycosis, topical agents are used to supplement the treatment of disinfection baths. In severe cases, the doctor will prescribe medicine for the fungus.
Only the doctor can choose the exact drug after the test. The listed drugs are effective against yeasts and molds. The cream should be applied to the previously cleansed and dry skin twice a day. In this case, the agent must not only be applied to the affected skin, but also the healthy epidermis around the infected nail.
In order to avoid the spread of spores to healthy skin areas, it is necessary to additionally use preservatives. For this, use hydrogen peroxide, potassium permanganate or iodine solutions.
The funds in the form of varnish remain on the nail plate for a long time, ensuring effective destruction of pathogenic microflora and preventing further spread of fungal spores.
The treatment of nail fungus takes a long time. On average, the course of treatment lasts 9 months. Only after healthy nails have grown can you stop using the drug.
Before applying varnish, nails must be steamed, filed and degreased with alcohol solution or alcohol-containing napkins.
In the initial stages of ringworm of small nails, you can use a strong antifungal ointment. The drug is used after foot baths and pedicures. In order for the drug to penetrate deeper into the nail plate, it must be carefully polished to eliminate all microcracks.
In the case of severe onychomycosis or recurrence of the disease, the doctor may prescribe medication. They have a systemic effect on the entire body and help fight pathogenic microflora from within.
Remove nails

The nail on the little finger is small, almost invisible, and grows quickly, so the doctor can recommend a thorough treatment-removing the nail infected with the fungus. The process itself is quick and painless. There are also special kits containing uric acid, which can soften the nail and promote its independent separation from the nail bed.
After removing the nails, apply a special ointment and bandage on the fingers. After 5-7 days, a crusty skin will form under the bandage, which can be removed. The nails will grow back in about a month. It has always been necessary to use antifungal drugs to prevent re-infection.
The benefit of removing the nail plate is to minimize the risk of contamination of healthy nails. This allows you to get rid of the fungus in one day, but you have to wait until the nails have fully grown back. On average, the nail on the little finger fully recovers within 3-4 months.
Folk remedies
It is recommended to use folk remedies for milder forms of fungi. They help prevent the spores of the pathogenic microbial flora from spreading to healthy fingers, so they are a perfect complement to medical treatments.
- Lemon juice can effectively remove yeast. It can be used for Candida-infected nails. For this, covering the nails with lemon juice twice a day is sufficient.
- Fungus paste will help overcome this disease. To prepare this product, you must mix a teaspoon of baking soda with an equal amount of water and apply it to your nails. The compression should be maintained for half an hour, and the procedure should be repeated twice a day until the symptoms disappear completely.
- The basis of folk remedies for fungi consists of bathing. They can be prepared with iodine, baking soda, salt, hydrogen peroxide, boric acid powder or herbs. For each liter of water, you must take one tablespoon of the selected product. You must take a bath for 20 minutes before going to bed every day.
The folk remedy perfectly prepares the skin and nails for the application of fungal ointment. As an independent medicine, they are ineffective, so you cannot rely entirely on traditional medicine.
How to avoid being infected?
Preventing fungal infections comes down to personal hygiene. Always use slippers when going to public showers and swimming pools. Do not use other people’s towels or wear other people’s shoes.
If a person has ever been infected with foot fungus, antifungal ointments should be used regularly for prevention. For this, it is sufficient to apply them to the skin 1-2 times a week.
Foot hygiene plays an important role in preventing fungal infections. It is necessary to wash your feet with antiseptic or tar soap every day, wear only socks made of natural fabrics, and choose comfortable shoes made of breathable materials.
Fungus between the toes: symptoms (photos), the best ointments and folk remedies
Of all types of fungal diseases, foot lesions are the most common.
One type of foot fungus is fungus between the toes. This disease can cause severe itching and peeling of the skin, which can cause severe discomfort. You can get fungus in any public place with high humidity.
This type of fungal disease occurs in adults and children.
Causes of disease development
Fungus between the toes is a type of foot mycosis. The disease is contagious and difficult to treat. The treatment process can last for several months.
The fungus between the toes develops due to the following reasons:
- Failure to observe foot hygiene;
- Go to public places with high humidity;
- Wear someone else's shoes;
- Use someone else's towel.
The easiest way to get infected is to go to a public shower without adequate protective equipment. In shared shower rooms, gym locker rooms, or even in a moderate temperature sauna, if there are no separate slippers, fungal infections between the toes will occur. Symptomatic photos will not suspect the nature of peeling.
Ignoring personal hygiene can lead to fungus between the toes of children and adults. Lack of proper foot care can cause sweat and dirt to accumulate in the space between the fingers.
This is a favorable breeding ground for fungi.
Because certain pathogens always exist in the human body, even without contact with potential sources of infection, the fungal microbiota on the skin will occur.
Fungus on the skin between the feet and toes is a highly contagious fungal infection. If someone is infected, you may get sick when trying on someone else's shoes. This is because the fungal spores will attach to the inner surface of the shoe and easily attach to healthy skin.

Even if a family member is fighting a fungal infection, you may get sick. In fact, the spores of the pathogenic microbial flora will attach to all objects in contact with the affected skin. Spores persist in carpet piles, towels, and surfaces in bathrooms and showers. The slightest contact with these objects is enough to allow the spores to penetrate into healthy skin.
However, not everyone gets the fungus from using someone else’s towel or showering. Factors that cause the development of fungus between the toes:
- Decreased overall and local immunity;
- Damage to the skin of the feet;
- Sweat a lot;
- Long-term use of antibiotics;
- Frequent stress
- Wear shoes that are too tight;
- A disease that causes poor blood circulation in the lower limbs.
Long-term medication and frequent stress will weaken the body, making it vulnerable to various bacteria and fungi. Wearing narrow shoes will cause local blood circulation to be blocked, thereby reducing the immunity of the feet. This creates favorable conditions for the rapid development of pathogenic microbial flora.
Fungi in the foot and interdigital space are particularly susceptible to people with diabetes, cardiovascular disease, and varicose veins in the lower extremities. All of these pathologies can lead to deterioration of local metabolic processes and destruction of cellular immunity, thereby increasing the risk of infection with fungi.
Factors that trigger infections include wearing very tight shoes made of low-quality materials, synthetic socks and excessive sweating. All these have created a favorable environment for the development of pathogenic microbial communities. With a lot of sweating, the process of increasing the number of fungi accelerates because this microbiome likes hot and humid environments.

Folk remedies
Traditional medicine knows how to remove the fungus between the toes. For this reason, it is recommended to use trays and solutions to treat the skin.
- Pour 2 bags of boric acid into a basin of water, and then place your feet for 20 minutes. Apply every other day.
- An effective mycosis bath-4 liters of hot water, 2 tablespoons of soda water, salt and iodine. Take 15 minutes, then lubricate your feet with ointment.
- You can use the application in a soda solution containing vinegar. When preparing the product, dissolve a teaspoon of soda and vinegar in half a cup of water. Then dip the cotton swab into the solution and treat the skin thoroughly.
For daily foot hygiene, it is recommended to use tar or laundry soap. They can perfectly remove oil from the skin and have a weak anti-fungal effect.
Preventing the development of fungus between the toes is a thorough hygiene of the feet. Be sure to bring your own rubber slippers to the swimming pool, gym and sauna. You should not use other people's hygiene products or try on strangers' shoes because they may contain fungal spores.
In summary, we can conclude that foot fungus is an extremely dangerous disease. The consequences of this disease can be extremely detrimental to human health. Do not self-administer medication to avoid complications.















